19-Year-Old German Women POWs Reached a U.S. Camp with Bone Infection
War does not end the moment weapons fall silent. For many, its consequences arrive later—quietly, carried inside the body, unnoticed until someone finally looks closely enough. In the chaotic final phase of the Second World War and its uncertain aftermath, a small group of nineteen-year-old German women arrived at a U.S.-run prisoner camp carrying more than exhaustion, fear, and confusion. They carried a medical condition so advanced that it left seasoned military doctors deeply unsettled.
What shocked the physicians was not only the severity of the illness, but how long it had gone untreated—and how easily it could have remained invisible.
This article examines the journey of these young prisoners, the circumstances that led to their condition, and what their arrival revealed about the hidden medical toll of war, especially on those least expected to bear it.
Too Young for the Weight They Carried
At nineteen, life is usually measured in plans, not survival. Yet by the final months of the war, age had lost much of its meaning. Germany’s collapsing infrastructure had pulled adolescents into roles once reserved for adults. Many young women served as assistants, messengers, or support staff, while others were displaced civilians swept up in mass detentions as front lines dissolved.

When Allied forces advanced rapidly, large numbers of people were detained under provisional classifications. Some were soldiers. Some were auxiliaries. Others were simply in the wrong place at the wrong time.
Among them were several nineteen-year-old women who appeared, at first glance, physically small but otherwise unremarkable. They were transported with other detainees to a U.S.-administered camp intended as a temporary holding site.
Nothing in their paperwork suggested a medical emergency.
Their bodies told a different story.
The Long Journey Before the Camp
To understand the condition that shocked U.S. doctors, one must look beyond the camp gates.
These young women had endured weeks—sometimes months—of movement through disrupted regions. Transportation was inconsistent. Medical services were overwhelmed or nonexistent. Minor injuries, which would have been routine in peacetime, were often ignored in favor of simply staying alive.
A small wound. Persistent pain. Swelling that never fully subsided.
In a functioning healthcare system, such symptoms would trigger immediate attention. In a collapsing one, they became background noise.
The women learned to endure.
Arrival at the U.S. Camp
When the transport vehicles finally reached the U.S.-run facility, processing was swift. Names were recorded. Basic examinations were conducted. The focus was on classification and containment, not detailed diagnostics.
Initially, the women did not stand out.
They walked on their own. They followed instructions. They did not ask for help.
Only after several days did camp staff begin to notice subtle signs: limping that worsened at night, fevers that returned repeatedly, visible discomfort during routine activities. When questioned, the women minimized their symptoms.
They had learned that drawing attention rarely helped.
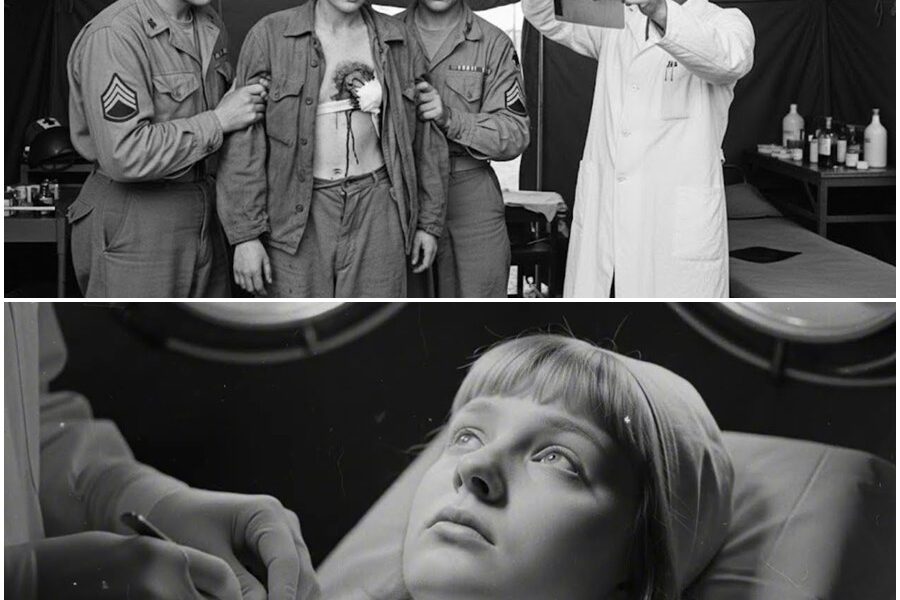
The Medical Examination That Changed Everything
Eventually, one of the women collapsed during a work detail. That incident prompted a more thorough medical evaluation—not only of her, but of others who shared similar complaints.
What the doctors found was alarming.
The condition was advanced, deeply rooted, and unmistakable. It had not developed overnight. It had progressed quietly over time, likely originating from untreated injuries or infections sustained long before captivity.
The physicians were not shocked because they had never seen such cases.
They were shocked because they were seeing them in teenagers.
Why the Diagnosis Was So Disturbing
The condition itself was serious, but what troubled the medical staff most was what it implied:
-
The women had lived with significant pain for an extended period
-
Their access to medical care had been delayed repeatedly
-
Warning signs had been present but ignored by necessity
In other words, this was not just a medical issue. It was evidence of systemic breakdown.
For military doctors trained to treat acute battlefield injuries, encountering advanced, untreated conditions in such young patients was deeply unsettling. It challenged assumptions about who suffered most during the war.
Youth Does Not Mean Resilience
There is a persistent myth that young bodies recover easily. That youth compensates for hardship.
The doctors knew better.
While younger patients often have stronger baseline health, prolonged neglect can undo that advantage. Delayed treatment allows conditions to advance silently, becoming harder—not easier—to address.
In these cases, age had not protected the women.
It had merely masked the severity of what was happening inside them.
Silence as a Survival Strategy
When asked why they had not reported their symptoms earlier, the women gave similar answers.
They did not believe help was available.
They had seen others turned away.
They feared being labeled difficult or uncooperative.
And above all, they had learned that endurance was safer than complaint.
This silence was not apathy. It was adaptation.
The Camp’s Medical Staff Responds
Once the seriousness of the condition was recognized, the camp’s medical team shifted priorities. Work assignments were adjusted. Monitoring increased. Treatment plans were established within the limits of available resources.
The doctors documented what they could. They consulted each other. They expressed concern—not only for these patients, but for how many others might be carrying similar conditions undetected.
This was not an isolated case.
It was a warning.
The Bigger Picture of Wartime Neglect
These women’s condition highlighted a broader truth about the final phase of the war: systems were collapsing faster than suffering could be recorded.
Medical records were lost. Clinics closed. Supply lines failed. In that environment, countless injuries went untreated—not because no one cared, but because no one could keep up.
Young women, often perceived as less likely to be seriously harmed, slipped through the cracks.
Their pain was real, but invisible.
Why Official Records Say So Little
You will not find extensive documentation of this episode in official military archives. The focus of records was on logistics, transfers, and demobilization.
Individual medical cases rarely made headlines unless they affected operational readiness.
As a result, stories like this survived primarily through later recollections, medical notes, and fragmented testimony.
Absence of documentation does not mean absence of reality.
The Emotional Impact on the Doctors
Several medical staff later described the experience as unsettling not only professionally, but personally. Treating young patients whose conditions reflected months of neglect forced them to confront the quieter consequences of war.
These were not combat wounds.
They were time wounds—damage done slowly, invisibly, by delay.
Recovery Was Not Immediate
Treatment did not offer instant relief. Healing took time, rest, and continued care—resources not always plentiful in temporary camps.
For some of the women, recovery extended well beyond their period of detention. The condition followed them into postwar life, shaping their physical limits and their memories.
The war stayed with them—not as noise, but as ache.
Why This Story Still Matters
This is not a story about blame. It is a story about awareness.
It reminds us that:
-
The youngest are not immune to long-term harm
-
Medical neglect can be unintentional and still devastating
-
Some of war’s worst injuries do not happen in combat
These women were not statistics. They were individuals whose bodies recorded what official histories overlooked.
The Quiet Legacy
Today, their story challenges simplified narratives of resilience and recovery. It asks us to look beyond visible wounds and consider what goes untreated when systems fail.
Because sometimes, the most shocking discoveries are not found on battlefields—but in examination rooms, when someone finally takes the time to look.
Note: Some content was generated using AI tools (ChatGPT) and edited by the author for creativity and suitability for historical illustration purposes.